Common Conditions
Chronic Obstructive Pulmonary Disease(COPD)
What Is COPD?
Chronic obstructive pulmonary disease (COPD) is a serious lung disease that makes it harder and harder for you to breathe. COPD includes chronic bronchitis, emphysema, or both. These two conditions make it difficult to breathe:

COPD can cause coughing that produces large amounts of mucus (a slimy substance), wheezing, shortness of breath, chest tightness, and other symptoms.
Cigarette smoking is the leading cause of COPD. Most people who have COPD smoke or used to smoke. Long-term exposure to other lung irritants, such as air pollution, chemical fumes, use of charcoal in cooking, or dust, also may contribute to COPD.
What are the signs and symptoms of COPD?
The signs and symptoms of COPD include:
- An ongoing cough or a cough that produces large amounts of mucus (often called “smoker’s cough”)
- Shortness of breath, especially with physical activity
- Wheezing (a whistling or squeaky sound when you breathe)
- Chest tightness
These symptoms often occur years before the flow of air into and out of the lungs declines. However, not everyone who has these symptoms has COPD. Likewise, not everyone who has COPD has these symptoms.
Some of the symptoms of COPD are similar to the symptoms of other diseases and conditions. Your doctor can determine if you have COPD.
If you have COPD, you may have frequent colds or flu. If your COPD is severe, you may have swelling in your ankles, feet, or legs; a bluish color on your lips due to low levels of oxygen in your blood; and shortness of breath.
COPD symptoms usually slowly worsen over time. At first, if symptoms are mild, you may not notice them, or you may adjust your lifestyle to make breathing easier. For example, you may take the elevator instead of the stairs.
Over time, symptoms may become bad enough to see a doctor. For example, you may get short of breath during physical exertion.
How severe your symptoms are depends on how much lung damage you have. If you keep smoking, the damage will occur faster than if you stop smoking. In severe COPD, you may have other symptoms, such as weight loss and lower muscle endurance.
How COPD progresses?
COPD is progressive. This means it gets worse over time. At first, some people think their breathing problems are just part of getting older. Or they think they are getting “out of shape.” But these symptoms may actually be a sign of something much more serious.
COPD gradually worsens. It progresses from mild to moderate, and then severe. COPD can’t be cured, but it can be treated at any stage. It is important to talk to your doctor about ways to manage your COPD.
If you have mild COPD, you may:
- Feel a little short of breath after you work hard or do high-energy activities (like biking or climbing stairs)
- Cough a lot and sometimes cough up mucus (phlegm)
If you have moderate COPD, you may:
- Feel short of breath when you walk up a hill
- Have trouble doing chores like taking out the garbage
- Cough a lot and sometimes cough up mucus (phlegm)
- Need a few weeks to get better from a lung infection like a bad cold
- Cut back on activities you enjoy
If you have severe or very severe COPD, you may:
- Get short of breath during low-energy activities like showering or getting dressed
- Not be able to work or take part in simple activities you enjoy
- Cough a lot and sometimes cough up mucus (phlegm)
- Need a few weeks to get better from a lung infection like a bad cold
- Have trouble breathing day and night
People with severe or very severe COPD often need oxygen therapy.
COPD can’t be cured, but it can be treated at any stage. Your doctor is your best source for treatment information. With the right treatment and lifestyle changes, you may improve your breathing today and every day.
How COPD differs from other breathing problems?
COPD is often mistaken for other breathing problems. So it’s important to understand what COPD is and what it isn’t. COPD is not asthma. COPD and asthma are two different conditions, but are often confused with one another. The chart below helps explain the differences between COPD and asthma. Make sure you know the differences so that you can partner better with your doctor.
The Different Between COPD and Asthma
| Factors | Asthma | COPD |
|---|---|---|
| Age when it starts |
|
|
| Triggers/Causes |
|
|
| Symptoms |
|
|
| Airflow |
|
|
How is COPD diagnosed?
Your doctor will diagnose COPD based on your signs and symptoms, your medical and family histories, and test results.
He or she may ask whether you smoke or have had contact with lung irritants, such as air pollution, chemical fumes, or dust. If you have an ongoing cough, your doctor may ask how long you’ve had it, how much you cough, and how much mucus comes up when you cough. He or she also may ask whether you have a family history of COPD.
Your doctor will examine you and use a stethoscope to listen for wheezing or other abnormal chest sounds. You also may need one or more tests to diagnose COPD.
The main test for COPD is spirometry. Lung function tests measure how much air you can breathe in and out, how fast you can breathe air out, and how well your lungs can deliver oxygen to your blood. Other lung function tests, such as a lung diffusing capacity test, may also be used. Chest x-ray and especially CT thorax scan can show up COPD.
How is COPD treated?
COPD has no cure yet. However, treatments and lifestyle changes can help you feel better, stay more active, and slow the progress of the disease. Quitting smoking is the most important step you can take to treat COPD. Other treatments for COPD may include medicines, vaccines, pulmonary rehabilitation, oxygen therapy, surgery, and managing complications. The goals of COPD treatment are to:
- Relieve your symptoms
- Slow the progress of the disease
- Improve your exercise tolerance (your ability to stay active)
- Prevent and treat complications
- Improve your overall health
Medicines
Bronchodilators
Bronchodilators relax the muscles around your airways. This helps open your airways and makes breathing easier. Depending on how severe your disease is, your doctor may prescribe short-acting or long-acting bronchodilators. Short-acting bronchodilators last about 4 to 6 hours and should be used only when needed. Long-acting bronchodilators last about 12 hours or more and are used every day.
Most bronchodilators are taken using a device called an inhaler. This device allows the medicine to go right to your lungs. Not all inhalers are used the same way. A spacer device may be recommended to be used with inhaler for patients.
If your COPD is mild, your doctor may only prescribe a short-acting inhaled bronchodilator. In this case, you may only use the medicine when symptoms occur.
If your COPD is moderate or severe, your doctor may prescribe regular treatment with short- and long-acting bronchodilators.
Latest Combination Inhalers use both beta-agoinst and anti-cholinergic agents in the same inhaler such as Anoro, Ultibro, Spiolto. Both agents can open up airways better and for longer period of time.
Inhaled Glucocorticosteroids (Steroids)
Inhaled steroids are used for some people who have moderate or severe COPD. These medicines may reduce airway inflammation (swelling). Your doctor may ask you to try inhaled steroids for a trial period of 6 weeks to 3 months to see whether the medicine is helping with your breathing problems in COPD.
There is also the latest inhaler which combines beta-agoinst, anti-cholingeric and steroid in the same inhaler called Trelegy, Trimbow.
Vaccines
Flu Shots
The flu (influenza) can cause serious problems for people who have COPD. Flu shots can reduce your risk for the flu. Talk with your doctor about getting a yearly flu shot.
Pneumococcal Vaccine
This vaccine lowers your risk for pneumococcal pneumonia and its complications. People who have COPD are at higher risk for pneumonia than people who don’t have COPD. Talk with your doctor about whether you should get this vaccine. The most recent pneumonia vaccine is Prevenar 13.
Pulmonary Rehabilitation
Pulmonary rehab is a medically supervised program that helps improve the health and well-being of people who have lung problems. Rehab may include an exercise program, disease management training, and nutritional and psychological counselling. The program aims to help you stay more active and carry out your day-to-day activities.
Your rehab team may include doctors, nurses, physical therapists, respiratory therapists, exercise specialists, and dietitians. These health professionals work together and with you to create a program that meets your needs.
Oxygen Therapy
If you have severe COPD and low levels of oxygen in your blood, oxygen therapy can help you breathe better. For this treatment, you’re given oxygen through nasal prongs or a mask. You may need extra oxygen all the time or just sometimes. For some people who have severe COPD, using extra oxygen for most of the day can help them:
- Do tasks or activities, while having fewer symptoms
- Protect their hearts and other organs from damage
- Sleep more during the night and improve alertness during the day
- Live longer
Surgery
In rare cases, surgery may benefit some people who have COPD with evidence of bullae. Surgery usually is a last resort for people who have severe symptoms that have not improved from taking medicines.
What is the role of maintenance therapy in COPD and how does it work?
If you have COPD, you have a chronic disease. That means it doesn’t go away and it may need to be managed with daily treatment. This is where maintenance therapy comes in. When taken as directed, maintenance therapy helps control COPD. So you can breathe better, longer. Unlike rescue medicines that you take just when you need them, maintenance medicines have to be taken every day to work properly.
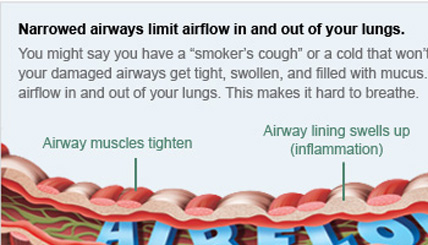
With COPD your airways are damaged. They become tight and filled with mucus. This blocks the flow of air into and out of your lungs. Maintenance medicines help keep your airways open, so you can breathe better all day. They are taken on a regular schedule to help you manage your COPD. This is why these medicines must be taken every day as directed to feel the full effects. You will lose these medicines’ benefits if you do not take them as directed.
Maintenance medicines work over time and their effects are long-lasting. This is why you may not “feel” them working right away. When it is time for you to take your dose the medicine from your last dose is still working. So the effects of maintenance medicines are not always so easy to notice.
Some people think that once they feel better, they can stop taking their daily medicines. The fact is, if you are breathing better, it means your maintenance medicine is working. Remember: to keep breathing better you must keep taking this medicine every day as directed by your doctor.
National Heart Lung and Blood Institute.What is COPD?
http://www.nhlbi.nih.gov
Accessed December 10, 2009.
http://www.spiriva.com/consumer/index.jsp
Accessed December 10, 2009.
