Common Conditions
Chronic Cough
Introduction
Persistent cough is one of the most frequent symptoms which present to the General Practitioner. It is estimated approximately 24,263,000 visits to the clinic in the United States in 1991[1] involved chronic cough. The prevalence of chronic cough among the non-smoking adult population ranges from 14 – 23%[2,3]. It is therefore very important to know the causes of persistent cough and its management.
Persistent cough may be defined as persistent cough of more than three weeks’ duration. The cause of persistent cough may be divided into two broad groups: patients who have a normal chest X-ray and patients who have an abnormal chest X-ray. This article will describe the causes of persistent cough in a patient with a normal chest X-ray.
Approach to Persistent Cough
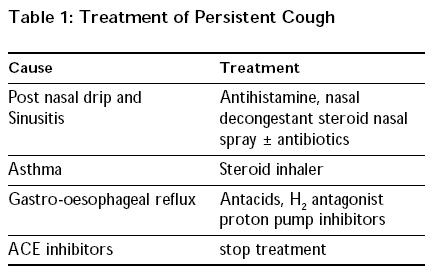
A simple algorithm in the approach to persistent cough is shown in Figure 1. The commonest causes of persistent cough are asthma, post-nasal drip and gastro-oesophageal reflux disease (GERD)[4]. Post viral cough may also cause persistent cough. Angiotensin converting enzyme (ACE) inhibitors such as Lisinopril, Enalapril may also cause cough in up to 46% of patients[5,6] in some studies. The cause of persistent cough and its treatment is summarised in Table 1.
Asthma
Relevant questions to ask for asthma are a history or family history of asthma or atopy. Nocturnal cough or cough exacerbated by exercise, or by other common asthma triggers such as changes in weather, may also be symptoms of asthma.
The investigation of choice for asthma is a Pulmonary Function Test. Spirometry may demonstrate an obstructive ventilatory defect with an improvement in FEV1 (Forced expiratory Volume in I second) of more than 13% post bronchodilator. An example of a spirometry test which demonstrates asthma is shown in Figure 2.
Home peak flow monitoring which demonstrates a variation in peak flow readings of more than 15% may also diagnose asthma. It is important to make sure that the patient is able to perform and record peak flow readings precisely if this technique is used.
Persistent cough caused by asthma responds well to an inhaled corticosteroid7. It is important to make sure that the patient is able to use the inhaler device well.
Post-Nasal Drip
Post-nasal drip is another common cause of persistent cough. This is diagnosed if there is a history of rhinitis and examination of the nares demonstrates mucosal inflammation of the inferior turbinates. Post-nasal drip responds well to an antihistamine and nasal decongestant. Patients may benefit from a mild steroid nasal spray if an allergic component is present. Sinusitis should be considered if the patient’s symptoms persist. A sinus X-ray and rhinoscopy by an ENT surgeon may be helpful.
Figure: Algorithm for Persistent Cough
Figure: Treatment of Persistent Cough
Figure: Pulmonary Function Test which shows mild airway obstruction with reversibility
Post Vial or Infective Cough
Gastro-oesophasteal Reflux
Gastro-oesophageal reflux disease (GERD) may cause persistent cough[8,9]. Relevant questions such as if the cough is worse at night or there is a history of peptic ulcer disease may suggest gastrooesophageal reflux. However, when GERD is the cause of the cough, there may be no gastrointestinal symptoms in up to 75% of patients[9]. The investigation of choice is oesophageal pH monitoring which may be unpleasant and costly[9]. An empirical trial of either an H2 antagonist or proton pump inhibitor for eight weeks with response to treatment would suggest this diagnosis[8].
An Aid to Diagnosis of Persistent Cough
Previous studies have shown that up to 61.1% of patients with persistent cough may have more than one cause for coughing[11]. It is therefore important to identify more than one cause of cough, and treatment should be aimed at these causes simultaneously.
Example 1
Mr RS, a 50-year-old executive, had a history of recurrent sinus disease. Despite adequate treatment by his doctor, he had persistent cough for 8 years. There was no history of asthma or symptoms to suggest gastro-oesophageal reflux. Clinical examination was normal. Chest X-ray was normal. Pulmonary function testing was normal. CT sinus demonstrated pansinusitis (Figure 3).
Despite sinus surgery, his cough persisted. HRCT of the thorax demonstrated bronchiectasis of the left lower lobe (Figure 4). Diagnosis: Bronchiectasis and sinusitis. He was treated with an inhaled corticosteroid and bronchodilators. His cough resolved.
Example 2
Mrs LCY, a 55-year-old teacher, had a history of depression and was on anti-depressant treatment.
Figure: CT Sinus which shows pansinusitis
She had persistent cough for two months with retching, especially at night. She also had a history of sinusitis. Clinical examination: tenderness in the epigastric area, with no other abnormalities detected. Chest X-ray was normal. Sinus X-ray was normal. Pulmonary function testing was normal.
Diagnosis: gastro-oesophageal reflux and post nasal-drip with a history of depression. Treatment: She was treated with proton pump inhibitors for gastro-oesophageal reflux, an antihistamine and a decongestant nasal spray for the postnasal drip. Her cough resolved.
Example 3
Mrs VB, a 42-year-old housewife had persistent cough for two months. She was a smoker of 5 cigarettes per day for 20 years and had a history of sinusitis. Clinical examination: Lungs: wheeze at the right base. Chest X-ray was normal. Sinus Xray: maxillary sinusitis.
Pulmonary function testing: FEV1 1.93L (71% predicted), FVC 2.98L(94% predicted), ratio FEV1 / FVC 64.8% with an improvement in FEV1 post-bronchodilator of 16% (Figure 2).
Figure: HRCT Thorax demonstrating bronchiectasis of the left lower lobe
Provisional diagnosis: asthma exacerbated by smoking and recurrent sinusitis (Figure 5). The patient’s cough persisted despite adequate treatment for asthma with inhaler therapy and sinusitis. The patient was further investigated. HRCT Thorax showed tree-in-bud parenchymal abnormalities (Figure 6). Tuberculosis culture of the sputum isolated mycobacterium tuberculosis.
Figure: Sinus X-ray demonstrating maxillary sinusitis with a fluid level in the right maxillary antrum
Figure: HRCT Thorax demonstrating parenchymal ‘tree-in-bud’ abnormalities of endobronchial tuberculosis
Final diagnosis: Endobronchial tuberculosis, asthma and sinusitis. Treatment: The patient completed six months of anti-tuberculous therapy and was also treated with nasal decongestants and an inhaled corticosteroid. Her cough resolved.
Conclusion
The commonest causes of persistent cough are asthma, post-nasal drip and gastrooesophageal reflux disease. Treatment is aimed at the cause which may have multiple causes.
REFERENCES
- Shappert SM (1991). National ambulatory medical care summary: 1991 summary. Adv Data 23 0, 1-16.
- Di Pede C, Viegi G, Quechenboss JJ et al. Respiratory symptoms and risk factors in Arizona population sample of Anglo and Mexican-American whites.Chest 1991; 99: 916-22.
- Irwin RS, Curley FJ (1991). The treatment of cough: a comprehensive review.Chest 1991; 99: 1477-84.
- Diagnosis and management of chronic persistent dry cough. Chung KF, Lalloo NG Postgrad Med J 1996 Oct 72: 594-8.
- Prevalence of persistent cough during long term enalopril treatment: controlled study versus nifedipine. Yeo WW, Foster G, Ramsay LE. Q J Med 1991 Sept 80: 763-70.
- High prevalence of persistent cough with angiotensin converting enzyme inhibitors in Chinese. Woo KS, Nicholls MG. Br J Chin Pharmacol 1995 Aug 40: 141-4.
- Outcome of cough variant asthma treated with inhaled steroids. Cheriyan S, Greenberger PA, Patterson R. Ann Allergy 1994 Dec 73: 478-8010.
- Chronic cough and gastro-oesophageal reflux: a doubleblind placebo-controlled study with omeprazole. KiIjander TO, Salomae ER, Hietanen EK, Terho EO. Eur Resp J 2000 Oct: 633-8.
- Anatomical diagnostic protocol in evaluating chronic cough with specific reference to gastro-oesophageal reflux disease. Irwin RS, Madison JM. Am J Med 2000 Mar 108 suppl 4a : 126S-13 OS.
- Chronic persistent cough and gastro-oesophageal reflux Ing AJ, Ngu MC, Breshi AB. Thorax 1991 Jul 46:479-83. 11. Palombini BC, Villanova CAC, Aranjo E, Cameiro D, Stolz DP, Palombibi CO. Pathogenic Triad in Chronic Cough. Asthma, post-nasal drip and gastro-oesophageal reflux disease. Chest 1991; 116: 279-84.